Eczematous cheilitis is a condition that can be described as a living nightmare for those who suffer from it. Imagine waking up every day with painfully cracked, dry, and inflamed lips that not only affect your appearance but also make it difficult to eat, drink, or even speak without discomfort. This distressing skin condition, characterized by inflammation of the lips due to eczema, poses significant challenges for individuals seeking relief.
While there may be various causes of eczematous cheilitis, such as allergies and irritants, its symptoms are unmistakable. The affected area may appear red, swollen, scaly, and may even develop blisters or crusts. It can be an isolating experience for those affected by this condition as they struggle to find effective treatments that provide long-term relief.
In this article, we will explore the common causes of eczematous cheilitis and delve into the signs and symptoms that accompany it. We will also discuss how healthcare professionals diagnose this condition and the treatment options available. Additionally, we will share real-life case studies and personal experiences to shed light on what it’s like living with eczematous cheilitis. Finally, we will provide additional resources and support for individuals seeking guidance on managing their condition effectively.
By understanding the complexities of eczematous cheilitis and exploring evidence-based approaches to treatment and management strategies, we hope to create a sense of belonging for those afflicted by this challenging condition.
Eczematous cheilitis is a type of inflammation of the lips that is characterized by dryness, cracking, and redness. It is a common condition that can affect people of all ages and genders. The exact cause of eczematous cheilitis is not fully understood, but it is believed to be multifactorial in nature.
There are several factors that can contribute to the development of eczematous cheilitis. One possible cause is allergic contact dermatitis, which occurs when an allergen comes into contact with the lips and triggers an immune response. Common allergens include certain lip balms, toothpaste ingredients, and cosmetic products.
Another potential cause of eczematous cheilitis is irritant contact dermatitis. This occurs when the lips are repeatedly exposed to irritating substances such as saliva, acidic foods or drinks, or harsh weather conditions. Individuals who frequently lick their lips or have a habit of biting their lips may be more prone to developing this condition.
In addition to these external factors, certain internal factors may also increase the risk of developing eczematous cheilitis. These include underlying medical conditions such as atopic dermatitis or food allergies. Stress and hormonal changes can also play a role in triggering flare-ups.
Treatment options for eczematous cheilitis aim to reduce inflammation and relieve symptoms. Non-pharmacological remedies such as avoiding known triggers and maintaining proper lip care hygiene are often recommended as initial steps. Moisturizing creams or ointments containing ingredients like petrolatum or ceramides can help restore moisture to the lips.
If symptoms persist or worsen despite these measures, topical corticosteroids may be prescribed by a healthcare professional for short-term use. In severe cases where there is significant inflammation or infection present, oral corticosteroids may be necessary.
Eczematous cheilitis is a common inflammatory condition affecting the lips. It can be caused by various factors, including allergens, irritants, and underlying medical conditions. Treatment involves identifying and avoiding triggers, maintaining proper lip care hygiene, and using moisturizing creams or ointments. In more severe cases, corticosteroids may be prescribed.
By incorporating these lifestyle modifications into their daily routine, individuals with eczematous cheilitis may experience relief from symptoms such as dryness, redness, and itching. However, it’s essential to consult with a healthcare professional before making any significant changes to one’s diet or skincare regimen.
Key Takeaways
- Eczematous cheilitis is a condition characterized by inflammation of the lips due to eczema, causing painful cracked, dry, and inflamed lips.
- Common triggers for eczematous cheilitis include allergies, irritants, and underlying medical conditions.
- Treatment options aim to reduce inflammation and relieve symptoms, including avoiding triggers and using moisturizing creams or ointments.
- Effective management strategies include seeking medical advice, applying moisturizing agents regularly, and addressing the underlying causes.
[bulkimporter_image id=’2′]
Definition and Overview of Eczematous Cheilitis
[bulkimporter_image id=’3′]
Common Causes of Eczematous Cheilitis
Common causes of inflamed and irritated lips often stem from external factors such as allergens, irritants, or environmental triggers. Eczematous cheilitis, a condition characterized by redness, dryness, and cracking of the lips, can be triggered by a variety of factors. Extensive research has been conducted to identify these common triggers and irritants. One of the main causes of eczematous cheilitis is contact allergy to certain substances. Common allergens include fragrances, preservatives in lip products, metals like nickel or cobalt found in jewelry or dental materials, and even specific food items such as citrus fruits or spices. Individuals who are sensitized to these allergens may develop an allergic reaction when they come into contact with them on their lips. Irritants also play a significant role in causing eczematous cheilitis. These include chemicals present in lip care products such as lip balms or lipsticks that can cause irritation and inflammation. Additionally, environmental factors like extreme weather conditions (such as cold winds or excessive sun exposure) can lead to dryness and chapping of the lips. Research suggests that individuals with underlying skin conditions like atopic dermatitis are more prone to developing eczematous cheilitis. The compromised skin barrier function in these individuals makes their lips more susceptible to external triggers. Common causes of eczematous cheilitis include contact allergies to substances like fragrances or metals, irritants present in lip care products, environmental factors like extreme weather conditions, and underlying skin conditions such as atopic dermatitis. It is important for individuals experiencing symptoms of eczematous cheilitis to identify and avoid these triggers to effectively manage their condition.[bulkimporter_image id=’4′]
Symptoms and Signs of Eczematous Cheilitis
Eczematous cheilitis is characterized by several distinct symptoms and signs. One common manifestation is dryness and chapping of the lips, which can lead to discomfort and difficulty in performing daily activities such as eating or speaking. Additionally, redness and swelling are often observed in affected individuals, indicating inflammation in the lip area. Finally, cracking and pain are frequently reported symptoms, further exacerbating the discomfort experienced by those with eczematous cheilitis. Overall, these symptoms contribute to the impairment of lip function and quality of life for individuals with this condition.Dryness and Chapping of the Lips
Dryness and chapping of the lips can cause discomfort and frustration for individuals affected by eczematous cheilitis. This condition is characterized by inflammation, redness, and scaling of the lips, which can lead to pain and difficulty in speaking or eating. To better understand this subtopic, it is essential to explore the causes and risk factors associated with dryness and chapping of the lips in eczematous cheilitis. 1) Environmental factors: Exposure to cold weather, wind, or dry air can contribute to lip dryness. 2) Allergens: Certain substances like cosmetics, toothpaste, or lip products can trigger an allergic reaction leading to chapped lips. 3) Poor oral hygiene: Neglecting proper lip care and not moisturizing regularly can worsen lip dryness. Fortunately, various treatment options are available for managing dryness and chapping of the lips in eczematous cheilitis. These include using emollients or medicated creams containing ingredients like corticosteroids or antifungal agents. Additionally, lifestyle modifications such as avoiding triggers and maintaining good oral hygiene practices play a crucial role in preventing further aggravation of symptoms.Redness and Swelling
Redness and swelling of the lips can cause significant discomfort and impairment in individuals affected by this condition, highlighting the need for effective management strategies. Eczematous cheilitis, a common form of lip inflammation, often presents with these symptoms. The redness and swelling can be attributed to an underlying inflammatory response triggered by various factors such as irritants, allergens, or infections. To effectively manage redness and swelling in eczematous cheilitis, treatment options focus on reducing inflammation and restoring skin barrier function. Topical corticosteroids are commonly prescribed to alleviate symptoms and reduce inflammation. Moisturizers containing ingredients like ceramides can help restore the damaged skin barrier while providing hydration. In severe cases, oral anti-inflammatory medications may be prescribed. Avoiding triggers such as certain foods or lip care products that may exacerbate symptoms is also recommended. Consulting with a healthcare professional is essential to determine the most appropriate treatment plan for individuals experiencing redness and swelling due to eczematous cheilitis.Cracking and Pain
Cracking and pain in the lips can cause significant discomfort and interfere with daily activities, emphasizing the need for effective management strategies. Eczematous cheilitis, a condition characterized by inflammation of the lips, often presents with symptoms such as redness, swelling, cracking, and pain. The causes of lip cracking in eczematous cheilitis are multifactorial and can include environmental factors, such as exposure to cold weather or wind, as well as irritants like certain foods or lip care products. Effective pain relief for cracked lips involves addressing the underlying causes and providing symptomatic relief. Moisturizing agents containing ingredients like petrolatum or beeswax can help restore moisture to the lips and alleviate dryness. Additionally, topical corticosteroids may be prescribed to reduce inflammation and provide pain relief. It is important to consult a healthcare professional for an accurate diagnosis and appropriate management plan for eczematous cheilitis.- Emotional sub-lists:
- Strategies to manage painful cracked lips effectively:
- Seeking medical advice promptly
- Applying moisturizing agents regularly
- The impact of cracked lips on daily life:
- Difficulty speaking or eating
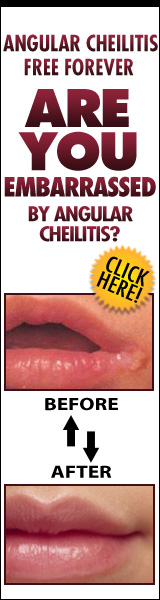
- Social embarrassment due to visible discomfort
[bulkimporter_image id=’5′]
Diagnosis of Eczematous Cheilitis
One important aspect in the diagnosis of eczematous cheilitis is identifying the underlying cause, which can be linked to a variety of factors including allergic reactions, irritants, or even nutritional deficiencies. According to a recent study published in the Journal of Dermatology, it was found that approximately 60% of patients diagnosed with eczematous cheilitis had a history of allergic contact dermatitis. Diagnosing eczematous cheilitis can pose some challenges due to its similarity with other lip conditions. The differential diagnosis methods used by dermatologists include thorough medical history taking, physical examination, patch testing for allergens, and laboratory tests. The first step in the diagnostic process is obtaining a detailed medical history from the patient. This includes information about any previous skin conditions or allergies, exposure to potential irritants or allergens such as cosmetics or dental products, and any recent changes in diet or medication. It is also important to inquire about symptoms such as dryness, cracking, redness, itching, and pain experienced on the lips. Physical examination plays a crucial role in diagnosing eczematous cheilitis. The dermatologist will carefully examine the lips for signs of inflammation such as erythema (redness), edema (swelling), scaling, and fissures (cracks). Additionally, they may assess if there are any accompanying symptoms on other parts of the body that could indicate an underlying systemic condition. Patch testing is another valuable tool used in diagnosing eczematous cheilitis. This involves applying small amounts of potential allergens onto patches that are then placed on the patient’s back for 48-72 hours. After this period, any positive reactions observed at the site where an allergen was applied can help identify specific triggers. Laboratory tests may be conducted if there is suspicion of nutritional deficiencies contributing to eczematous cheilitis. Blood tests can measure levels of essential vitamins and minerals, such as iron or vitamin B12, which are important for skin health. Diagnosing eczematous cheilitis requires a comprehensive approach that takes into account the patient’s medical history, physical examination findings, patch testing results, and laboratory tests if needed. By utilizing these differential diagnosis methods, dermatologists can accurately identify the underlying cause of eczematous cheilitis and provide appropriate treatment options.[bulkimporter_image id=’6′]
Treatment Options for Eczematous Cheilitis
The treatment options for eczematous cheilitis consist of emollients and moisturizers, topical steroids and anti-inflammatory medications, as well as the avoidance of triggers and irritants. Emollients and moisturizers play a crucial role in maintaining hydration and restoring the skin barrier function. Topical steroids are commonly used to reduce inflammation and itching, while anti-inflammatory medications may also be prescribed for severe cases. Additionally, identifying and avoiding triggers such as certain foods or environmental factors can help prevent flare-ups and promote healing.Emollients and Moisturizers
Emollients and moisturizers play a crucial role in the management of eczematous cheilitis, providing much-needed hydration to soothe and alleviate the discomfort associated with this condition. When selecting an emollient, it is important to consider its composition and suitability for lip application. Emollients containing ingredients such as petrolatum, shea butter, or beeswax are often recommended due to their occlusive properties that help retain moisture in the skin. Additionally, moisturizers with added humectants like glycerin or hyaluronic acid can attract water molecules to the lips and further enhance hydration. It is worth noting that some individuals may find relief by using alternative treatments such as natural oils (e.g., coconut oil) or lip balms specifically formulated for sensitive skin. However, evidence supporting their efficacy remains limited, and it is advisable to consult a healthcare professional before trying any alternative therapies.Topical Steroids and Anti-inflammatory Medications
Topical steroids and anti-inflammatory medications serve as potent weapons in the battle against the discomfort and inflammation associated with eczematous cheilitis, providing targeted relief to affected individuals. Topical corticosteroids are commonly prescribed due to their ability to reduce inflammation and suppress the immune response involved in this condition. These medications work by inhibiting the production of inflammatory mediators and preventing the infiltration of immune cells into affected areas. They have shown efficacy in managing symptoms such as itching, redness, and scaling. However, it is important to note that long-term use of topical corticosteroids can lead to adverse effects such as skin thinning and increased susceptibility to infections. Therefore, alternative therapies like calcineurin inhibitors or barrier creams may be considered for individuals who require prolonged treatment or are concerned about potential side effects. Further research is needed to explore the effectiveness and safety profile of these alternative options in managing eczematous cheilitis.Avoidance of Triggers and Irritants
Avoidance of triggers and irritants is crucial in managing the discomfort and inflammation associated with eczematous cheilitis. To minimize symptoms, individuals should identify and avoid specific triggers that exacerbate their condition. This may include allergens such as certain foods, cosmetics, or environmental factors like extreme temperatures or dry air. Implementing a consistent and gentle skin care routine is also essential to prevent further irritation. Dermatologists often recommend using mild cleansers specifically formulated for sensitive skin and avoiding harsh soaps or scrubs. Additionally, moisturizing regularly with fragrance-free emollients can help maintain skin hydration and integrity. Protecting the lips from exposure to wind, sun, or other potential irritants by using lip balms containing SPF or natural oils can aid in symptom control. By diligently avoiding triggers and following appropriate skincare practices, individuals can effectively manage eczematous cheilitis symptoms and improve their overall quality of life.- Identify and avoid specific triggers
- Implement a consistent and gentle skincare routine
- Protect the lips from exposure to irritants
[bulkimporter_image id=’7′]
Lifestyle and Home Remedies for Eczematous Cheilitis
To alleviate the symptoms of eczematous cheilitis, individuals can adopt simple yet effective measures in their daily routine. Apart from avoiding triggers and irritants, lifestyle and home remedies can play a crucial role in managing this condition. Natural remedies and dietary changes are two key aspects that individuals can incorporate to help improve their symptoms. One effective natural remedy for eczematous cheilitis is the application of coconut oil. Coconut oil has been shown to have anti-inflammatory properties and can help moisturize the lips, reducing dryness and flakiness. Another option is shea butter, which contains vitamins A and E that promote skin healing. Applying a thin layer of shea butter on the lips several times a day can provide relief. In terms of dietary changes, individuals should focus on consuming foods rich in omega-3 fatty acids such as fatty fish (salmon, mackerel) or plant-based sources like chia seeds or flaxseeds. Omega-3 fatty acids have anti-inflammatory properties that may help reduce inflammation associated with eczematous cheilitis. Additionally, it is important to stay hydrated by drinking plenty of water throughout the day. This helps keep the body and lips adequately moisturized. To summarize these natural remedies and dietary changes for eczematous cheilitis management:| Natural Remedies | Dietary Changes |
|---|---|
| Coconut oil | Foods rich in omega-3 |
| Shea butter | fatty acids |
[bulkimporter_image id=’8′]
Prevention of Eczematous Cheilitis
One crucial aspect in managing eczematous cheilitis is implementing preventive measures. By taking proactive steps, individuals can reduce the frequency and severity of flare-ups, leading to better overall management of the condition. Here are some preventive measures that can be taken:- Avoid triggers: Identifying and avoiding triggers that worsen eczematous cheilitis is essential. Common triggers include irritants like certain lip products, fragrances, and allergens such as certain foods or environmental factors like cold weather. By eliminating exposure to these triggers, individuals can minimize the risk of developing flare-ups.
- Moisturize regularly: Keeping the lips well-moisturized is important in preventing eczematous cheilitis. Applying a hypoallergenic lip balm or ointment regularly helps to maintain moisture and prevent dryness and cracking.
- Protect from sun exposure: Sunburns can exacerbate symptoms of eczematous cheilitis. Therefore, it is advisable to protect the lips from excessive sun exposure by using a lip balm with SPF or wearing a wide-brimmed hat when outdoors for extended periods.
- Practice good oral hygiene: Maintaining good oral hygiene is crucial in preventing secondary infections that can worsen eczematous cheilitis. Regularly brushing teeth and gently cleaning around the mouth area helps to remove bacteria that may contribute to inflammation.
[bulkimporter_image id=’9′]
Complications and Long-term Effects of Eczematous Cheilitis
Implementing preventive measures and effectively managing eczematous cheilitis can help individuals avoid complications and minimize the long-term effects of this condition, ensuring a smoother journey towards healthier lips. Complications may arise if the condition is left untreated or inadequately managed. These complications include secondary bacterial or fungal infections, which can further exacerbate the inflammation and lead to more severe symptoms. In addition, recurrent episodes of eczematous cheilitis can cause chronic lip swelling and discomfort, making it challenging for individuals to eat, speak, or perform daily activities. Proper management of eczematous cheilitis involves identifying and avoiding triggers that may aggravate the condition. Common triggers include irritants such as certain lip balms, toothpaste ingredients like sodium lauryl sulfate, certain foods or food additives, environmental factors like cold weather or wind exposure, and stress. By eliminating these triggers from one’s routine or environment, individuals can significantly reduce the recurrence of symptoms. Furthermore, regular use of emollients and moisturizers specifically designed for sensitive lips can help maintain proper hydration and prevent dryness that often leads to cracking and inflammation. In severe cases where over-the-counter treatments are ineffective, medical intervention may be necessary. This could involve prescription-strength corticosteroids or other topical medications to alleviate symptoms. The psychological impact of eczematous cheilitis should not be overlooked either. Individuals with this condition may experience embarrassment or self-consciousness due to visible lip redness, scaling, crusting, or blistering. They might also face social stigma or difficulty in interpersonal relationships because others may misinterpret their lip appearance as a contagious disease. Therefore, providing emotional support alongside medical treatment is crucial in addressing any concerns related to body image issues and improving overall well-being. By implementing preventive measures such as trigger avoidance strategies and proper management techniques like regular moisturization with appropriate products, individuals with eczematous cheilitis can minimize complications and long-term effects. Addressing the psychological impact of this condition is equally important in ensuring a holistic approach to care.[bulkimporter_image id=’10’]
When to Seek Medical Help for Eczematous Cheilitis
Seeking timely medical help is essential for individuals with persistent or worsening symptoms of inflamed and cracked lips, as it may indicate a more severe case of eczematous cheilitis that requires professional intervention. Eczematous cheilitis can have a significant impact on daily life and self-esteem, making it crucial to seek appropriate medical attention. When dealing with eczematous cheilitis, the condition can cause discomfort and pain, affecting one’s ability to eat, drink, speak, and even smile. The constant itchiness and inflammation may make it difficult to carry out regular activities without discomfort. Furthermore, the visible symptoms of cracked and red lips can significantly impact an individual’s self-esteem and confidence in social situations. If the initial management strategies such as avoiding triggers, using emollients or lip balms do not provide relief within a reasonable time frame (usually a few days), seeking medical help is advisable. Additionally, if there are signs of infection such as pus-filled blisters or spreading redness around the affected area, prompt medical attention should be sought. Medical professionals specializing in dermatology or oral medicine can accurately diagnose eczematous cheilitis by conducting a thorough examination of the affected area. They may also perform tests to rule out other potential causes or identify specific triggers. Once diagnosed, they can provide appropriate treatment options tailored to each individual’s case. When experiencing persistent or worsening symptoms of eczematous cheilitis that impact daily life and self-esteem despite initial management attempts, seeking medical help is crucial. Timely intervention from healthcare professionals specializing in this field ensures accurate diagnosis and targeted treatment plans to alleviate discomfort and improve quality of life for individuals affected by this condition.[bulkimporter_image id=’11’]
FAQs about Eczematous Cheilitis
When to Seek Medical Help for Eczematous Cheilitis has provided us with valuable information about identifying the signs and symptoms that warrant medical attention. Now, let’s delve into some frequently asked questions (FAQs) about eczematous cheilitis to further enhance our understanding of this condition. One common question is regarding the treatment options available for eczematous cheilitis. It is important to note that the approach to treatment may vary depending on the severity and underlying cause of the condition. In mild cases, self-care measures such as avoiding triggers, keeping lips moisturized, and using over-the-counter lip balms containing emollients or petroleum jelly may suffice. However, if these measures do not provide relief or if the condition worsens, it is advisable to seek medical help. Another misconception surrounding eczematous cheilitis pertains to its contagious nature. It is important to clarify that eczematous cheilitis itself is not contagious. The inflammation and dryness of the lips are a result of various factors such as allergies, irritants, or underlying skin conditions like atopic dermatitis. Therefore, there is no need for concern about spreading the condition through casual contact. Additionally, individuals often wonder whether eczematous cheilitis can be permanently cured. While complete cure may not always be possible due to its multifactorial nature, effective management can significantly reduce symptoms and improve quality of life. Working closely with a healthcare professional who specializes in dermatology can help determine suitable treatment options tailored to individual needs. Understanding common misconceptions about eczematous cheilitis and being aware of available treatment options are crucial in effectively managing this condition. By seeking appropriate medical help when necessary and following recommended treatments diligently, individuals can find relief from symptoms associated with eczematous cheilitis.[bulkimporter_image id=’12’]
Research and Studies on Eczematous Cheilitis
Research and studies on the condition characterized by inflammation and dryness of the lips have provided valuable insights into understanding its multifactorial nature. Eczematous cheilitis is a complex condition that can be caused by various factors, including allergies, irritants, infections, and underlying medical conditions. To better understand this condition and develop effective treatment strategies, researchers have utilized different research methods and evaluated the effectiveness of various treatments.- Epidemiological studies: Researchers have conducted epidemiological studies to determine the prevalence and incidence of eczematous cheilitis in different populations. These studies help identify risk factors associated with the condition, such as age, gender, occupation, or exposure to certain substances.
- Patch testing: Patch testing is an important tool used in diagnosing eczematous cheilitis caused by allergy or contact dermatitis. It involves applying small amounts of potential allergens to patches placed on the skin to identify specific triggers that may be causing the lip inflammation.
- Histopathological analysis: Histopathological analysis involves examining tissue samples from affected lips under a microscope. This helps researchers identify specific cellular changes indicative of eczematous cheilitis and differentiate it from other lip conditions.
- Treatment effectiveness evaluation: Research studies have evaluated the effectiveness of various treatment options for eczematous cheilitis, including topical corticosteroids, emollients, antifungal agents, or immunomodulators like tacrolimus or pimecrolimus. These studies assess treatment outcomes based on objective measures such as symptom improvement, reduction in inflammation, or healing time.
[bulkimporter_image id=’13’]
Case Studies and Personal Experiences
Case studies and personal experiences provide valuable insights into the manifestations, challenges, and potential treatments of eczematous cheilitis, a condition characterized by inflammation and dryness of the lips. These individual accounts offer real-life examples of how this condition can affect individuals and how they navigate through the daily challenges it presents. One case study published in the Journal of Dermatological Case Reports described a 35-year-old woman who presented with chronic inflammation and scaling of her lips. The patient reported significant discomfort and distress due to social embarrassment caused by the visible symptoms. The case study highlighted the importance of accurate diagnosis and appropriate treatment to alleviate symptoms and improve quality of life. Another case report documented a 42-year-old man who experienced recurrent episodes of eczematous cheilitis triggered by certain foods. Through careful observation and dietary modifications, he was able to identify specific triggers that exacerbated his symptoms. This case emphasized the significance of individualized management strategies tailored to each patient’s unique triggers. In addition to case studies, personal experiences shared on online forums have provided insights into coping strategies employed by individuals with eczematous cheilitis. Some individuals have found relief through regular lip care routines consisting of gentle cleansing, moisturizing, and sun protection. Others have experimented with various natural remedies or alternative therapies such as herbal ointments or acupuncture. Overall, these case studies and personal experiences shed light on the diverse manifestations of eczematous cheilitis as well as coping strategies employed by those affected. However, it is important to note that individual responses may vary, necessitating personalized approaches in treatment management plans for optimal outcomes. Further research is needed to explore effective interventions for this challenging condition.[bulkimporter_image id=’14’]
Conclusion: Living with Eczematous Cheilitis
Transitioning from the previous subtopic of case studies and personal experiences, we now shift our focus to the conclusion: living with Eczematous Cheilitis. Living with this chronic condition can be challenging, but through various coping strategies and support systems, individuals can find ways to manage their symptoms and improve their quality of life.- Acceptance: Accepting the reality of living with eczematous cheilitis is an essential step towards finding peace and making necessary adjustments in one’s daily routine. Acknowledging that it is a long-term condition allows individuals to seek appropriate treatment and adopt coping mechanisms that best suit their needs.
- Self-care: Prioritizing self-care is crucial for managing eczematous cheilitis effectively. This includes maintaining good oral hygiene, avoiding triggers such as certain foods or environmental factors, and using lip balms or ointments recommended by healthcare professionals to soothe dryness and inflammation.
- Seeking support: Connecting with others who are also dealing with eczematous cheilitis can provide a sense of belonging and understanding. Online communities, support groups, or forums provide opportunities for sharing experiences, seeking advice, and gaining emotional support from individuals who have firsthand knowledge of the challenges associated with this condition.
- Professional help: Seeking professional help from dermatologists or allergists who specialize in skin conditions like eczematous cheilitis is vital for effective management of symptoms. These experts can provide personalized treatment plans tailored to individual needs, which may include medications such as topical steroids or immunomodulators.
[bulkimporter_image id=’15’]
Additional Resources and Support for Eczematous Cheilitis
BEGINNING OF THE SENTENCE:
Exploring additional resources and support networks can offer individuals with eczematous cheilitis a lifeline in their journey towards managing this chronic condition. Eczematous cheilitis, also known as lip eczema, is a distressing and often painful skin condition that affects the lips. It can cause discomfort, embarrassment, and impact one’s quality of life. However, by accessing various resources and support systems, individuals can find solace in knowing they are not alone in their struggles. One valuable resource for those living with eczematous cheilitis is online community forums. These platforms provide a safe space for individuals to connect with others who share similar experiences and challenges. Here, they can discuss coping strategies, exchange advice on treatment options, and seek emotional support from people who truly understand what it feels like to live with this condition. Community forums foster a sense of belonging and create opportunities for individuals to form meaningful connections with others facing the same difficulties. In addition to online communities, there are several other resources available that can assist those dealing with eczematous cheilitis. Dermatologists specialized in lip conditions can provide expert guidance on treatment options and management strategies tailored specifically to each individual’s needs. Moreover, patient education materials such as brochures or websites dedicated to lip-related dermatological conditions offer comprehensive information about the causes of eczematous cheilitis, potential triggers to avoid, and recommended skincare routines. Seeking professional counseling or therapy may be beneficial for individuals struggling emotionally due to the impact of eczematous cheilitis on their daily lives. Therapists trained in dealing with chronic conditions can help patients develop coping mechanisms to manage stressors related to their condition effectively. Overall, finding additional resources and support networks is crucial for individuals living with eczematous cheilitis. The combination of community forums where experiences are shared, professional guidance from dermatologists, and emotional support through counseling or therapy can empower individuals to navigate the challenges of this chronic condition with more confidence and resilience.[bulkimporter_image id=’16’]