Angular cheilitis is a dermatological condition characterized by inflammation and fissuring at the corners of the mouth. This article aims to provide an understanding of the different types of angular cheilitis, namely mild, severe, recurring, chronic, idiopathic, and bilateral. By examining these variations in detail, readers will gain insight into the diverse manifestations of this condition. The objective and informative nature of this article seeks to enlighten readers on the subject matter, while maintaining a rhythm and flow in writing that appeals to a wide audience.
Key Takeaways
- Symptoms of Angular Cheilitis include redness, swelling, pain, and fissures at the corners of the mouth.
- Treatment options for Chronic Angular Cheilitis include topical antifungal or antibacterial creams, moisturizing creams or ointments, and oral medications for infections or underlying conditions.
- Idiopathic Angular Cheilitis can be caused by infections, nutritional deficiencies, habits, and immune system issues, and treatment aims to address the underlying cause.
- Bilateral Angular Cheilitis affects both sides of the mouth and can be caused by nutritional deficiencies, poor oral hygiene, allergies, denture use, and immunocompromised conditions. Treatment focuses on symptom relief and healing.
Mild Angular Cheilitis
Mild angular cheilitis is characterized by slight redness, dryness, and cracking at the corners of the mouth. This condition can be caused by a variety of factors including fungal or bacterial infections, nutritional deficiencies, poor oral hygiene, or excessive saliva buildup. Symptoms may include discomfort or pain when opening the mouth wide, difficulty in eating or speaking, and occasionally bleeding.
To treat mild angular cheilitis, there are several options available. First and foremost is maintaining good oral hygiene practices such as regular brushing and flossing to prevent bacteria from accumulating in the affected area. Avoidance of irritants like spicy foods and acidic beverages can also help relieve symptoms. Over-the-counter antifungal creams or ointments containing ingredients like clotrimazole or miconazole can be applied topically to combat fungal infections.
Preventing mild angular cheilitis primarily involves addressing underlying causes. Ensuring a balanced diet rich in vitamins B2 (riboflavin) and B3 (niacin) can help prevent nutritional deficiencies that contribute to this condition. Additionally, individuals with braces should maintain proper oral hygiene to minimize saliva buildup in the corners of the mouth.
While home remedies for mild angular cheilitis might not provide complete resolution on their own, they can aid in symptom relief. Applying petroleum jelly or lip balm to keep the area moisturized helps alleviate dryness and cracking. Aloe vera gel has soothing properties which may also provide some relief.
Severe Angular Cheilitis
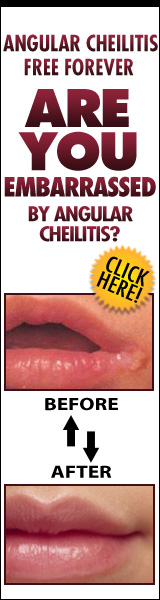
Severe angular cheilitis is characterized by pronounced inflammation, deep cracks, and ulceration at the corners of the mouth. It is a more advanced form of angular cheilitis and can significantly impact an individual’s quality of life. The condition may lead to pain, discomfort, difficulty eating and speaking, and social embarrassment.
Treatment options for severe angular cheilitis aim to address the underlying causes and relieve symptoms. Antifungal or antibacterial creams may be prescribed to combat infections. Topical corticosteroids can help reduce inflammation and promote healing. In some cases, oral antifungal or antibiotic medications may be necessary.
Causes of severe angular cheilitis include factors such as poor oral hygiene, nutritional deficiencies (especially in vitamins B2, B6, B12), ill-fitting dentures or braces that cause excessive moisture accumulation at the corners of the mouth, immunosuppression (e.g., HIV/AIDS), and systemic conditions like diabetes or hypothyroidism.
Prevention strategies for severe angular cheilitis involve maintaining good oral hygiene practices such as regular brushing and flossing. Adequate nutrition with a balanced diet rich in vitamins is also essential. Avoidance of irritants like lip licking or biting can help prevent exacerbation of symptoms.
Complications of severe angular cheilitis may include secondary bacterial infections or chronic inflammation leading to scarring. Long-term effects can vary depending on individual circumstances but can significantly impact one’s self-esteem and overall well-being.
The impact of severe angular cheilitis on quality of life should not be underestimated. Individuals with this condition may experience difficulties in social interactions due to embarrassment or self-consciousness about their appearance. Seeking appropriate treatment options early on can help alleviate symptoms and improve overall quality of life.
| Treatment Options | Causes & Risk Factors | Prevention Strategies |
|---|---|---|
| – Antifungal/antibacterial creams – Topical corticosteroids – Oral medications (antifungal/antibiotics) |
– Poor oral hygiene – Nutritional deficiencies – Ill-fitting dentures or braces – Immunosuppression (e.g., HIV/AIDS) – Systemic conditions (diabetes, hypothyroidism) |
– Good oral hygiene practices – Adequate nutrition with balanced diet rich in vitamins B2, B6, and B12 – Avoidance of lip licking or biting |
| Complications & Long-Term Effects | Impact on Quality of Life | |
| – Secondary bacterial infections – Chronic inflammation leading to scarring |
– Social embarrassment – Difficulties in social interactions – Self-esteem issues |
Recurring Angular Cheilitis
Recurring angular cheilitis, characterized by repeated episodes of inflammation and cracking at the corners of the mouth, poses a challenge in terms of management and prevention. This condition can cause discomfort and embarrassment for those affected, making it important to understand its causes, symptoms, treatment options, prevention measures, and home remedies.
Causes:
- Microorganisms: Fungal or bacterial infections are commonly associated with recurring angular cheilitis.
- Nutritional deficiencies: Deficiencies in iron, zinc, riboflavin (vitamin B2), or vitamin B12 can contribute to the development of this condition.
- Allergies: Certain substances like lip balms or oral care products may trigger allergic reactions leading to recurring angular cheilitis.
- Persistent moisture: Excessive saliva production or constantly licking the lips can create a moist environment that promotes fungal growth.
Symptoms:
- Redness and inflammation at the corners of the mouth
- Painful cracks or fissures that may bleed
- Dryness and tightness in the affected area
- Formation of crusts or scabs
Treatment Options:
- Antifungal or antibacterial creams prescribed by a healthcare professional
- Topical corticosteroids to reduce inflammation
- Oral antifungal medications if an underlying fungal infection is suspected
- Nutritional supplements to address any deficiencies contributing to the condition
Prevention Measures:
- Maintaining good oral hygiene by brushing teeth regularly and using alcohol-free mouthwash
- Avoiding excessive lip licking and keeping lips moisturized with non-irritating lip balm
- Treating any underlying medical conditions like diabetes that may increase susceptibility to recurring angular cheilitis
- Avoiding triggers such as allergenic substances found in certain cosmetics or oral care products
Home Remedies:
- Applying petroleum jelly or beeswax-based lip balm to keep the lips moisturized
- Using a clean cotton swab to apply diluted tea tree oil or honey to the affected area for their antibacterial properties
- Consuming a balanced diet rich in vitamins and minerals to support overall skin health
- Avoiding spicy, acidic, or salty foods that can irritate the cracked corners of the mouth
Chronic Angular Cheilitis
Chronic angular cheilitis is a persistent condition characterized by long-term inflammation and cracking at the corners of the mouth, which requires comprehensive management strategies. This condition can be caused by various factors, including nutritional deficiencies, fungal or bacterial infections, allergic reactions, and skin conditions such as eczema. The symptoms of chronic angular cheilitis typically include redness, swelling, pain, and fissures at the corners of the mouth. In severe cases, bleeding and crusting may also occur.
There are several treatment options available for chronic angular cheilitis. Topical antifungal or antibacterial creams may be prescribed to address underlying infections. Moisturizing creams or ointments can help soothe dry skin and promote healing. In some cases, oral medications may be necessary to control infections or manage underlying conditions. It is important to maintain good oral hygiene practices such as regular brushing and flossing to prevent further irritation.
Prevention tips for chronic angular cheilitis include maintaining a balanced diet rich in vitamins and minerals to prevent nutritional deficiencies that can contribute to this condition. Avoidance of irritants like saliva pooling in the corners of the mouth or excessive licking of lips is also recommended. Regularly applying lip balm with sun protection factor (SPF) can help protect the delicate skin around the mouth from further damage.
If left untreated or improperly managed, chronic angular cheilitis can lead to complications such as secondary bacterial infections or scarring. Seeking professional medical advice is essential for proper diagnosis and treatment planning based on individual needs. By following appropriate management strategies and preventive measures, individuals affected by chronic angular cheilitis can experience relief from symptoms while reducing the risk of recurrence and potential complications associated with this condition.
Idiopathic Angular Cheilitis
The etiology of idiopathic angular cheilitis remains unclear, as it is often characterized by inflammation and cracking at the corners of the mouth without an identifiable cause. This condition is also known as perleche or commissural cheilitis. Idiopathic angular cheilitis can be a chronic and recurrent condition, causing discomfort and affecting the individual’s quality of life. Here are some important points to consider about this condition:
- Causes: The exact causes of idiopathic angular cheilitis are unknown. However, several factors have been suggested to contribute to its development, including fungal or bacterial infections, nutritional deficiencies (such as iron or vitamin B12 deficiency), drooling during sleep, ill-fitting dentures or dental appliances, lip licking or biting habits, and compromised immune system.
- Symptoms: The most common symptoms of idiopathic angular cheilitis include redness, swelling, tenderness, and fissuring at the corners of the mouth. In severe cases, there may be crusting, bleeding, pain while eating or talking, and secondary infection.
- Treatment options: Treatment for idiopathic angular cheilitis aims to address the underlying cause if identified. This may involve antifungal or antibacterial medications in case of infection. Topical corticosteroids may be prescribed to reduce inflammation. Good oral hygiene practices and keeping the affected area clean and dry are essential for effective management.
- Prevention measures: To prevent recurrence of idiopathic angular cheilitis episodes, maintaining good oral hygiene is crucial. Avoiding triggers such as lip biting or licking can also help prevent exacerbation of symptoms. Adequate nutrition with a balanced diet is essential to avoid nutritional deficiencies that could contribute to this condition.
- Complications: If left untreated or poorly managed, complications such as chronic inflammation, scarring at the corners of the mouth (which can alter facial aesthetics), secondary bacterial infections (such as cellulitis), and discomfort while eating or speaking can occur.
Bilateral Angular Cheilitis
Bilateral angular cheilitis is characterized by inflammation and cracking at the corners of both sides of the mouth, often without an identifiable cause. This condition can cause discomfort and affect a person’s appearance, leading to social and psychological distress. Understanding the causes, symptoms, diagnosis, treatment options, prevention strategies, and complications of bilateral angular cheilitis is crucial in managing this condition effectively.
Causes and risk factors of bilateral angular cheilitis can vary from individual to individual. Common causes include:
- Nutritional deficiencies: Deficiencies in iron, vitamin B12, or riboflavin can contribute to the development of bilateral angular cheilitis.
- Poor oral hygiene: Inadequate oral care can lead to bacterial or fungal infections that may result in this condition.
- Allergies: Contact allergies to certain substances such as lip balms or dental products can trigger inflammation at the corners of the mouth.
- Denture use: Ill-fitting or poorly maintained dentures can create an environment conducive for bacterial or fungal growth.
- Immunocompromised conditions: Individuals with weakened immune systems are more susceptible to developing bilateral angular cheilitis.
Symptoms and signs of bilateral angular cheilitis typically include redness, swelling, pain, dryness, and fissures at the corners of the mouth. These symptoms may be accompanied by itching or a burning sensation.
Diagnosis of bilateral angular cheilitis involves a thorough examination by a healthcare professional who will assess physical signs and symptoms. In some cases, additional tests may be necessary if an underlying medical condition is suspected.
Treatment options for bilateral angular cheilitis depend on its underlying cause but generally focus on alleviating symptoms and promoting healing:
| Treatment Options | Description |
|---|---|
| Topical creams | Antifungal or corticosteroid creams may be prescribed to reduce inflammation and combat infection. |
| Nutritional supplements | If a nutritional deficiency is identified, supplementation may be recommended to address the underlying cause. |
| Oral hygiene improvements | Regular brushing, flossing, and using appropriate lip care products can promote healing and prevent recurrence. |
Prevention strategies for bilateral angular cheilitis involve:
- Maintaining good oral hygiene practices.
- Avoiding exposure to known allergens or irritants.
- Ensuring proper denture fit and maintenance.
Complications of bilateral angular cheilitis are rare but can include secondary bacterial infections or chronic inflammation if left untreated. Long-term effects may include scarring or hyperpigmentation at the corners of the mouth.
Frequently Asked Questions
What are the common triggers or causes of mild angular cheilitis?
Mild angular cheilitis can be triggered by various factors. Prevention strategies include maintaining good oral hygiene, avoiding excessive lip licking and biting, and keeping the lips moisturized. Common misconceptions about its causes include blaming solely on vitamin deficiencies or infection. To manage symptoms, one should keep the affected area clean and dry, use a barrier cream or ointment, and apply topical antifungal or antibacterial treatments if necessary. Nutritional deficiencies may contribute to its development, but they are not always the sole cause. Over-the-counter treatments such as hydrocortisone creams or lip balms containing zinc oxide can effectively alleviate symptoms of mild angular cheilitis.
How long does it usually take for severe angular cheilitis to heal?
Severe angular cheilitis can take several weeks to heal, depending on the individual and the underlying cause. Treatment options may include topical antifungal or antibiotic creams, oral medications, or in severe cases, surgical intervention. Prevention methods such as maintaining good oral hygiene and avoiding excessive moisture around the mouth can help reduce the risk of recurrence. Complications of severe angular cheilitis may include scarring or secondary bacterial infections. The condition can have a significant impact on daily life, causing pain and discomfort while speaking, eating, or smiling.
Are there any home remedies or natural treatments for recurring angular cheilitis?
Natural remedies, homemade treatments, alternative therapies, herbal remedies, and self-care techniques can be considered for recurring angular cheilitis. These approaches aim to alleviate symptoms and promote healing. Some potential options include applying natural oils such as coconut oil or tea tree oil, using honey or aloe vera gel topically, practicing good oral hygiene, avoiding irritants like spicy foods or harsh cosmetics, and maintaining a healthy diet rich in vitamins and minerals. However, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Can chronic angular cheilitis be cured completely, or is it a lifelong condition?
Chronic angular cheilitis, a long-term condition characterized by inflammation and cracking at the corners of the mouth, can be managed but not completely cured. Treatment options for chronic angular cheilitis include topical antifungal or antibiotic creams, as well as oral medications in severe cases. To alleviate symptoms, lifestyle changes such as maintaining good oral hygiene, avoiding irritants like acidic foods and lip licking are recommended. Support and resources for individuals living with lifelong angular cheilitis are available through patient support groups and online forums. Exploring alternative therapies may provide long-term relief for some individuals.
Is there any known link between specific medications and the development of idiopathic angular cheilitis?
Medication-related causes of idiopathic angular cheilitis are not well-documented, but certain medications have been associated with the development of this condition. For instance, chronic use of inhaled corticosteroids has been linked to angular cheilitis. To prevent its occurrence, maintaining good oral hygiene and addressing underlying factors like nutritional deficiencies can be helpful. Management strategies involve keeping the affected area clean and dry, using topical antifungal or antibacterial creams, and avoiding irritants. Treatment options may include topical steroids or antifungal medications.