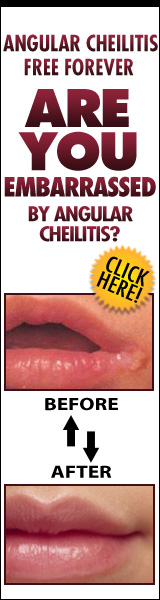
Angular cheilitis is a common condition characterized by inflammation and cracking at the corners of the mouth. It can cause pain, discomfort, and difficulty in performing basic oral functions such as eating and speaking. The exact cause of angular cheilitis is not always clear, but one possible factor that has been explored is fungal infection. This article aims to investigate the question: Is angular cheilitis fungal? Through an objective and evidence-based approach, we will examine the role of fungi in angular cheilitis, explore other potential causes of this condition, discuss available treatment options, and provide insights into preventing and managing angular cheilitis effectively. By presenting information in an academic style that is informative and devoid of personal bias or opinions, this article intends to serve as a reliable resource for individuals seeking knowledge about the relationship between fungal infections and angular cheilitis.
Key Takeaways
- Antifungal creams and ointments containing ingredients like miconazole or clotrimazole can effectively eradicate the fungal infection causing angular cheilitis.
- Natural remedies, such as a mixture of honey and coconut oil, can provide relief and promote healing for angular cheilitis due to their antimicrobial properties.
- Consulting with a healthcare professional is essential for a proper diagnosis, assessment of severity, and recommendation of appropriate interventions, including addressing underlying factors like vitamin deficiencies or immune system disorders.
- Preventing angular cheilitis requires maintaining good oral hygiene practices, keeping lips moisturized with lip balm, and avoiding habits like licking or biting the lips that can contribute to the condition.
Understanding Angular Cheilitis
Angular cheilitis, also known as perleche, is a condition characterized by inflammation and cracks at the corners of the mouth. The symptoms of angular cheilitis typically include redness, swelling, and painful fissures or cracks in the skin around the lips. Some individuals may also experience itching or burning sensations. The exact causes of angular cheilitis are not fully understood, but it is believed to be multifactorial.
One common cause of angular cheilitis is fungal infection. Candida albicans, a type of yeast commonly found on the skin and mucous membranes, is often associated with this condition. In some cases, an overgrowth of this fungus can lead to an infection in the corners of the mouth. Fungal infections thrive in moist environments, so factors such as excessive saliva production or drooling can contribute to their development.
Other potential causes of angular cheilitis include nutritional deficiencies, particularly deficiencies in iron or B vitamins. These deficiencies can weaken the immune system and make individuals more susceptible to infections like candidiasis. Additionally, conditions that cause chronic moisture or irritation around the mouth, such as ill-fitting dentures or lip-licking habits, can create an environment conducive to fungal growth.
In conclusion, while there are various causes for angular cheilitis including nutritional deficiencies and chronic moisture exposure; fungal infection caused by Candida albicans appears to be a significant factor in its development. Understanding these factors can help healthcare professionals diagnose and treat angular cheilitis effectively. It is important for individuals experiencing symptoms such as cracked lips or swelling at the corners of their mouth to seek medical attention for proper evaluation and treatment options tailored specifically to their needs.
The Role of Fungi in Angular Cheilitis
The presence of fungi plays a significant role in the development and progression of angular cheilitis. Angular cheilitis, also known as perleche, is a common condition characterized by inflammation and fissuring at the corners of the mouth. While multiple factors can contribute to its onset, fungal infection is often identified as a primary cause.
Fungal infections are commonly found in the oral cavity, with Candida species being the most frequently implicated pathogens in angular cheilitis. Candida albicans is particularly prevalent due to its ability to thrive in moist environments and its opportunistic nature. In individuals with compromised immune systems or poor oral hygiene, this fungus can overgrow and lead to an infection.
Treatment options for fungal-induced angular cheilitis focus on addressing the underlying fungal infection. Antifungal medications such as topical creams or ointments containing azole compounds are commonly prescribed. These agents work by inhibiting the growth of fungi and reducing inflammation. Additionally, maintaining good oral hygiene practices, including regular brushing and flossing, can help prevent fungal overgrowth.
It is important to note that while fungal infections are a common cause of angular cheilitis, other factors such as nutritional deficiencies, allergies, or excessive moisture can also contribute to its development. Therefore, proper diagnosis by a healthcare professional is essential for determining the most appropriate treatment approach.
In conclusion, fungi play a significant role in the occurrence of angular cheilitis. A thorough understanding of this association allows healthcare professionals to provide effective treatment options focused on addressing fungal infections. By adhering to good oral hygiene practices and utilizing antifungal medications when necessary, individuals suffering from angular cheilitis caused by fungi can find relief from their symptoms and promote healing.
Other Possible Causes of Angular Cheilitis
This discussion will explore other possible causes of angular cheilitis, such as nutritional deficiencies, irritation, and moisture. Nutritional deficiencies can contribute to the development of angular cheilitis, as certain vitamins and minerals play a key role in maintaining healthy skin. Irritation from factors like licking the lips or using irritating lip products can also lead to the condition. Additionally, excessive moisture in the corners of the mouth can create an environment that is conducive to fungal or bacterial overgrowth, further exacerbating angular cheilitis.
Nutritional Deficiencies
Nutritional deficiencies have been suggested as a potential cause for the development of angular cheilitis. This condition is characterized by redness, cracking, and inflammation at the corners of the mouth. While there is limited research specifically linking nutritional deficiencies to angular cheilitis, it is believed that certain vitamins and minerals play a role in maintaining healthy skin and mucous membranes. For example, deficiencies in iron, vitamin B12, riboflavin (vitamin B2), or zinc have been associated with oral manifestations such as angular cheilitis. These nutrients are essential for proper tissue repair and immune function. It is important to note that nutritional deficiencies alone may not be sufficient to cause angular cheilitis, but they may contribute to its development in individuals who are already predisposed due to other factors such as poor oral hygiene or weakened immune system. Further research is needed to fully understand the relationship between nutritional deficiencies and angular cheilitis.
Irritation and Moisture
Irritation and moisture can contribute to the discomfort and visible symptoms associated with angular cheilitis at the corners of the mouth. The causes of inflammation in this condition are varied, but irritation from saliva or food particles that accumulate in the corners of the mouth is a common factor. Excessive moisture in this area can create an environment conducive to bacterial or fungal growth, further exacerbating symptoms. The most common symptom of angular cheilitis is redness and swelling at the corners of the mouth, accompanied by pain or a burning sensation. Cracks and fissures may also develop, leading to discomfort when eating or speaking. It is important to address these factors to manage symptoms effectively and promote healing.
Treatment Options for Angular Cheilitis
One effective treatment option for angular cheilitis involves the application of antifungal creams or ointments, which work to eradicate the fungal infection causing the condition. These topical treatments typically contain active ingredients such as miconazole or clotrimazole, which have been shown to effectively combat fungal growth. When applied to the affected area, these antifungal agents target and eliminate the fungus responsible for angular cheilitis.
While antifungal creams or ointments are commonly used in treating angular cheilitis, it is important to note that there are other treatment options available. Some individuals may prefer natural remedies over medical interventions. For instance, applying a mixture of honey and coconut oil onto the affected area can provide relief from symptoms and promote healing due to their antimicrobial properties. Additionally, maintaining good oral hygiene and avoiding further irritation by using lip balms or moisturizers can help alleviate symptoms and prevent recurrence.
When considering treatment options for angular cheilitis, it is essential to consult with a healthcare professional who can assess the severity of the condition and recommend appropriate interventions. In some cases, underlying factors such as vitamin deficiencies or immune system disorders may contribute to the development of angular cheilitis. Addressing these underlying causes through dietary changes or supplementation may be necessary for complete resolution of symptoms.
Overall, while antifungal creams or ointments are an effective treatment option for angular cheilitis, individuals may also consider natural remedies and address any underlying factors contributing to their condition. Consulting with a healthcare professional will ensure proper diagnosis and guidance on suitable treatment approaches tailored to individual needs.
Preventing and Managing Angular Cheilitis
To effectively manage and prevent angular cheilitis, implementing proper oral hygiene practices and identifying any underlying factors contributing to the condition are crucial steps. Angular cheilitis is a common inflammatory condition characterized by redness, fissuring, and crusting at the corners of the mouth. It can be caused by a variety of factors, including fungal or bacterial infections, nutritional deficiencies, immune system disorders, or excessive moisture in the mouth.
Maintaining good oral hygiene is essential in preventing angular cheilitis. Regular brushing and flossing help remove plaque and bacteria from the mouth, reducing the risk of infection. It is also important to keep the lips moisturized with lip balm to prevent dryness and cracking. Avoiding habits that may exacerbate the condition, such as licking or biting the lips, can also help prevent recurrence.
Identifying and addressing any underlying causes of angular cheilitis is crucial for effective management. If a fungal infection is suspected, antifungal creams or ointments may be prescribed. In cases where bacterial infection is present, topical antibiotics can be used. Nutritional deficiencies should be addressed through dietary changes or supplementation if necessary.
In order to provide an overview of preventive measures for managing angular cheilitis effectively, a table highlighting common symptoms and prevention strategies could be useful:
| Common Symptoms | Prevention Strategies |
|---|---|
| Redness at corner of mouth | Maintain good oral hygiene |
| Cracking and fissuring | Keep lips moisturized with lip balm |
| Pain or discomfort | Avoid habits that worsen condition |
By following these preventive measures and seeking appropriate treatment when necessary, individuals can successfully manage and prevent angular cheilitis while maintaining optimal oral health.
Frequently Asked Questions
Can angular cheilitis be caused by a viral infection?
Angular cheilitis can be caused by a viral infection, among other factors. Viral causes of this condition include herpes simplex virus (HSV) and Epstein-Barr virus (EBV). Treatment options for angular cheilitis vary depending on the underlying cause. In cases where it is caused by a viral infection, antiviral medications may be prescribed to alleviate symptoms and promote healing. Additionally, maintaining good oral hygiene and applying topical creams or ointments can also help manage the condition.
Are there any home remedies that can effectively treat angular cheilitis?
Natural remedies can be used to effectively treat angular cheilitis. One such remedy is applying a mixture of honey and coconut oil to the affected area, as both have antimicrobial properties. Another option is using aloe vera gel, which has soothing and healing properties. Prevention measures include maintaining good oral hygiene, avoiding excessive moisture in the corners of the mouth, and ensuring a balanced diet rich in vitamins and minerals. These natural remedies and prevention measures can help alleviate symptoms and promote healing of angular cheilitis.
How long does it take for angular cheilitis to heal with treatment?
The healing time for angular cheilitis can vary depending on the severity of the condition and the effectiveness of treatment. In general, with appropriate treatment, it may take anywhere from a few days to several weeks for angular cheilitis to heal. Treatment options typically include topical antifungal or antibacterial creams, as well as keeping the affected area clean and moisturized. It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Can angular cheilitis be a sign of a more serious underlying health condition?
Angular cheilitis can sometimes be a sign of an underlying health condition. While fungal infections are commonly associated with angular cheilitis, there can be other causes as well. Some potential underlying causes include nutritional deficiencies, poor oral hygiene, allergic reactions, and autoimmune disorders. Medical treatments for angular cheilitis vary depending on the cause. Antifungal medications may be prescribed if a fungal infection is present, while other treatments may involve addressing any underlying health conditions or improving oral hygiene practices.
Is angular cheilitis contagious and can it be spread to others?
Angular cheilitis is not contagious and cannot be spread to others. It is an inflammatory condition that affects the corners of the mouth. While it may appear similar to a fungal infection, angular cheilitis is typically caused by a combination of factors such as dryness, irritation, or bacterial overgrowth. However, if there is an underlying fungal infection present, such as candidiasis, then it could potentially be transmitted to others through direct contact. Therefore, proper diagnosis and treatment are essential to prevent any potential transmission.
Conclusion
In conclusion, angular cheilitis is a condition that causes inflammation and cracking at the corners of the mouth. While fungal infections can contribute to this condition, it is not always the primary cause. Other factors such as bacterial infections, nutritional deficiencies, or excessive saliva can also play a role. Treatment options for angular cheilitis include antifungal creams, topical steroids, and lifestyle changes. Prevention and management techniques involve keeping the affected area clean and dry, maintaining good oral hygiene, and addressing underlying health issues.