Angular Cheilitis and Angioedema are two distinct dermatological conditions that can cause discomfort and distress for affected individuals. While they may sound similar, understanding the differences between these conditions is crucial for accurate diagnosis and appropriate treatment.
Angular cheilitis refers to the inflammation and cracking of the corners of the mouth, resulting in painful sores or fissures. On the other hand, angioedema involves swelling beneath the skin’s surface, typically affecting areas such as the lips, eyelids, or throat.
Differentiating these conditions based on location and appearance is essential in guiding proper management strategies. Furthermore, variations in duration and persistence can also provide valuable insights into their underlying causes.
This article aims to provide a comprehensive analysis of angular cheilitis and angioedema, delving into their distinctive causes and triggers. By exploring evidence-based research and authoritative sources, we will present a detailed account of symptoms, treatments, prevention methods, potential complications, and practical advice for individuals dealing with these conditions. Through this empathetic approach to serving others in need of medical guidance, we hope to empower patients with knowledge to navigate their journey towards optimal health.
Key Takeaways
- Angular cheilitis and angioedema are two different medical conditions with distinct symptoms, diagnosis, and treatment approaches.
- Angular cheilitis primarily affects the corners of the mouth, while angioedema can occur in various parts of the body, including the lips, face, throat, and extremities.
- The causes and triggers of angular cheilitis and angioedema differ, with angular cheilitis often being associated with fungal or bacterial infections, while angioedema can be triggered by allergic reactions, medications, or genetic factors.
- Treatment options for angular cheilitis include antifungal medications, while treatment for angioedema often involves the use of antihistamines. It is important to seek medical attention for both conditions, especially if symptoms worsen or complications arise.
Understanding Angular Cheilitis
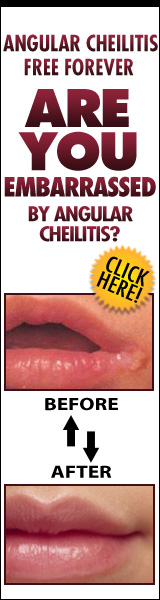
Angular cheilitis is a common inflammatory condition characterized by the presence of painful cracks or fissures at the corners of the mouth, often causing discomfort and embarrassment for those affected. The symptoms usually include redness, swelling, dryness, and irritation in the affected area. In some cases, there may also be a yellowish crust or discharge present.
Understanding the symptoms of angular cheilitis is crucial for accurate diagnosis and appropriate treatment. Apart from the physical manifestations mentioned above, patients may experience pain or tenderness when opening their mouths wide or during eating. These symptoms can significantly impact an individual’s ability to speak and eat comfortably.
Diagnosing angular cheilitis typically involves a thorough examination of the affected area by a dermatologist or healthcare professional. They will carefully assess the appearance of the cracks or fissures, ruling out other possible causes such as infections or allergies. In some cases, laboratory tests may be ordered to determine if there are any underlying conditions contributing to angular cheilitis.
It is important to note that angioedema is not synonymous with angular cheilitis but rather another distinct dermatological condition. Angioedema refers to localized swelling beneath the skin’s surface caused by an allergic reaction or genetic factors. While both conditions involve inflammation and can affect oral mucosal tissues, they have different causes and treatments.
In conclusion, understanding the symptoms and diagnosis methods associated with angular cheilitis is essential for effective management of this condition. By accurately identifying these signs and ruling out other potential causes, healthcare professionals can provide appropriate treatment options aimed at relieving discomfort and improving quality of life for individuals living with angular cheilitis.
Understanding Angioedema
Edema, a condition characterized by swelling in the deeper layers of the skin, is an important aspect to comprehend when exploring angioedema. Angioedema is a type of edema that affects the deep layers of the skin and mucous membranes. It is typically caused by an allergic reaction or hereditary factors. Differentiating symptoms between angular cheilitis and angioedema can be challenging, as they both involve swelling and inflammation in the affected areas.
One key difference lies in their location. Angular cheilitis primarily affects the corners of the mouth, causing redness, cracking, and sometimes ulceration. On the other hand, angioedema can occur anywhere on the body but commonly affects areas such as the lips, eyes, hands, feet, or genitals. The swelling associated with angioedema is often sudden and may be accompanied by itching or a burning sensation.
Misdiagnosis can occur when symptoms overlap between angular cheilitis and angioedema. For instance, some individuals with angioedema may initially be misdiagnosed with angular cheilitis due to similar symptoms around the mouth area. In order to differentiate between these conditions accurately, it is crucial for healthcare professionals to consider additional factors such as medical history, family history of allergies or hereditary angioedema (HAE), allergy testing results, and response to treatment.
Proper diagnosis is essential for effective management of both conditions. Treatment for angular cheilitis may involve addressing underlying causes such as nutritional deficiencies or fungal infections while applying topical creams or ointments to alleviate symptoms. In contrast, treatment for angioedema focuses on identifying triggers and avoiding allergens if possible. Medications like antihistamines or corticosteroids are often prescribed to reduce inflammation during acute episodes.
In conclusion,” Edematous conditions like angioedema require careful differentiation from other similar conditions like angular cheilitis. By understanding the distinct symptoms and considering individual medical histories, healthcare professionals can provide accurate diagnoses and appropriate treatment plans for patients suffering from these conditions.”
Differences in Location and Appearance
One distinguishing factor between these two conditions lies in the locations affected and their respective appearances. Angular cheilitis primarily affects the corners of the mouth, where the upper and lower lips meet. It is characterized by redness, swelling, and painful cracks or fissures in this area. The lesions may be accompanied by crusting or oozing of fluid. On the other hand, angioedema can affect various parts of the body including the face, lips, tongue, throat, hands, feet, and genitals. The skin in these areas becomes swollen and can appear pale or red.
In terms of appearance variations, angular cheilitis typically presents as localized inflammation at the corners of the mouth. The affected area may become dry and scaly with a distinct border separating it from healthy skin. Sometimes, small pustules or blisters may form on the surface. In contrast, angioedema causes more generalized swelling that extends beyond specific boundaries. The affected areas appear swollen and puffy without well-defined borders.
Location differences also play a role in differentiating these two conditions. Angular cheilitis is confined to the oral region whereas angioedema can occur in various parts of the body simultaneously or sequentially. Furthermore, angular cheilitis tends to persist for longer periods if left untreated while episodes of angioedema are often acute and self-limiting.
Understanding these location differences and appearance variations is crucial for accurate diagnosis and appropriate management of both angular cheilitis and angioedema. Dermatologists rely on precise terminology when describing symptoms to ensure effective communication with patients and colleagues. By considering these factors along with other clinical features such as medical history and laboratory test results, dermatologists can provide targeted treatments tailored to each individual’s condition.
Keywords: Location differences; Appearance variations
Variations in Duration and Persistence
Variations in the duration and persistence of angular cheilitis and angioedema can provide important insights for their diagnosis and management. Understanding these variations is crucial for healthcare professionals to effectively treat patients suffering from these conditions.
Angular cheilitis is a dermatological condition characterized by inflammation, redness, and cracking at the corners of the mouth. It can be caused by various factors such as fungal or bacterial infections, nutritional deficiencies, or excessive saliva accumulation. The duration of angular cheilitis varies from person to person depending on the underlying cause and individual immune response. In some cases, it may resolve within a few days with proper treatment, while in others, it may persist for several weeks or even months.
On the other hand, angioedema involves swelling beneath the skin’s surface and typically affects areas such as the lips, eyes, hands, feet, or genitals. It can be hereditary or acquired due to allergic reactions to certain medications or foods. The duration of angioedema episodes also varies widely among individuals. Some people experience short-lived episodes that last only a few hours before resolving completely. However, for others, swelling may persist for days or recur intermittently over an extended period.
The severity of both angular cheilitis and angioedema can have a significant impact on daily life. Persistent symptoms can cause discomfort while speaking or eating in the case of angular cheilitis and affect facial appearance in both conditions. Furthermore, recurrent episodes of angioedema can lead to anxiety and fear due to unpredictable swelling patterns.
To better understand variations in severity and their impact on daily life associated with these conditions, let us now explore a table comparing key aspects of angular cheilitis and angioedema:
| Aspect | Angular Cheilitis | Angioedema |
|---|---|---|
| Duration | Varies (days to months) | Varies (hours to days) |
| Recurrence | May persist or recur intermittently | May recur intermittently |
| Impact on daily life | Discomfort while speaking and eating | Facial appearance affected, anxiety and fear |
| Causes | Infections, nutritional deficiencies, saliva | Allergic reactions to medications or foods |
In conclusion, variations in the duration and persistence of angular cheilitis and angioedema play a crucial role in their diagnosis and management. Understanding these variations can help healthcare professionals provide appropriate treatment options tailored to each individual’s needs. By addressing the impact on daily life, empathetic care can be provided to patients dealing with these dermatological conditions.
Distinctive Causes and Triggers
Distinctive causes and triggers of these dermatological conditions are worth exploring to gain a comprehensive understanding of their etiology. Angular cheilitis and angioedema have different underlying causes, leading to distinct symptoms and treatment approaches.
Angular cheilitis is characterized by inflammation and cracking at the corners of the mouth. It is primarily caused by a combination of factors, including fungal or bacterial infections, nutritional deficiencies (such as iron, zinc, or riboflavin), and mechanical irritation from excessive drooling or lip licking. Certain predisposing factors like wearing ill-fitting dentures can also contribute to the development of angular cheilitis.
On the other hand, angioedema involves swelling beneath the skin’s surface, typically affecting the face, lips, tongue, throat, or extremities. It is often triggered by an allergic reaction mediated by histamine release. Allergens such as certain foods (e.g., shellfish or nuts), medications (e.g., nonsteroidal anti-inflammatory drugs), insect bites/stings, or environmental factors can initiate an immune response leading to angioedema.
Identifying and avoiding triggers is crucial in managing both conditions effectively. For angular cheilitis patients, addressing oral hygiene practices and correcting nutritional deficiencies through dietary changes or supplements may be necessary. Avoiding irritants like saliva contact with affected areas can help prevent further aggravation.
Angioedema treatment focuses on alleviating symptoms during acute episodes while preventing future attacks. Antihistamines are commonly prescribed to block histamine receptors and reduce swelling. In severe cases involving airway obstruction, prompt medical intervention with epinephrine may be required.
In conclusion, understanding the distinctive causes and triggers of angular cheilitis and angioedema provides valuable insights for healthcare professionals in diagnosing these conditions accurately and tailoring appropriate treatment plans for affected individuals. By considering individual patient circumstances and addressing both physical symptoms and emotional impact empathetically, healthcare providers can best serve those dealing with these dermatological conditions.
Treatment Approaches
Angular Cheilitis, a condition characterized by cracks or sores at the corners of the mouth, can be effectively treated with antifungal creams or ointments. These topical medications help to eliminate the fungal infection that often contributes to the development of angular cheilitis. On the other hand, for individuals suffering from Angioedema, a condition marked by sudden swelling beneath the skin’s surface, treatment options typically involve antihistamines or corticosteroids. These medications work to reduce inflammation and alleviate symptoms associated with angioedema.
Angular Cheilitis may require antifungal creams or ointments
Antifungal creams or ointments may be necessary for the treatment of angular cheilitis. This condition, characterized by inflammation and cracking at the corners of the mouth, can be caused by a variety of factors including fungal infections. While home remedies such as lip balms or honey may provide temporary relief, medical interventions are often required to effectively manage angular cheilitis.
Antifungal treatments work by targeting the underlying fungal infection that contributes to the development of angular cheilitis. These medications contain active ingredients like clotrimazole or miconazole, which inhibit the growth and spread of fungi. Applying antifungal creams or ointments directly to the affected areas helps eliminate fungal overgrowth and promotes healing.
It is important for individuals with angular cheilitis to consult a healthcare professional, such as a dermatologist, for an accurate diagnosis and appropriate treatment plan. In some cases, additional measures like addressing nutritional deficiencies or correcting oral hygiene practices may also be recommended to prevent recurrent episodes of angular cheilitis.
By following these evidence-based approaches and seeking medical guidance when needed, individuals can find relief from the discomfort associated with angular cheilitis and improve their overall quality of life.
Angioedema may be treated with antihistamines or corticosteroids
Treatment for angioedema often involves the use of antihistamines or corticosteroids, which act as a shield against the allergic reactions that trigger this condition, helping to alleviate symptoms and prevent further swelling. Antihistamines work by blocking histamine receptors in the body, reducing inflammation and itching associated with angioedema. They are commonly used for acute episodes of angioedema and can provide rapid relief. On the other hand, corticosteroids are powerful anti-inflammatory medications that suppress the immune system’s response to allergens, effectively reducing swelling in cases of severe or chronic angioedema. They may be prescribed when antihistamines alone are not sufficient or for long-term management of the condition. The effectiveness of these treatment options varies depending on the individual’s specific case and underlying causes of angioedema. It is important to consult with a healthcare professional to determine the most appropriate course of treatment for each patient.
Seeking Medical Attention
When experiencing angular cheilitis, it is recommended to seek medical attention if the condition persists or worsens despite home remedies and over-the-counter treatments. A dermatologist can provide a thorough examination, diagnose the underlying cause, and offer appropriate treatment options for effective management of angular cheilitis. On the other hand, angioedema may require immediate emergency medical care if it affects breathing or causes severe swelling in the face, lips, tongue, or throat. Seeking prompt medical attention is crucial to prevent potential complications associated with angioedema and ensure proper treatment is administered.
When to see a doctor for Angular Cheilitis
Seeking medical advice for angular cheilitis is essential, as early diagnosis and treatment can help prevent further complications and improve the overall well-being of the affected individual. Angular cheilitis is a common inflammatory condition characterized by painful cracks or sores at the corners of the mouth. It can be caused by various factors such as fungal or bacterial infections, nutritional deficiencies, or allergic reactions. Signs of severe angular cheilitis include excessive redness, swelling, bleeding, and difficulty in opening the mouth. To prevent angular cheilitis, it is important to maintain good oral hygiene, avoid licking lips excessively, use lip balms with SPF protection, and address any underlying health conditions. If you experience persistent symptoms or if the condition worsens despite self-care measures, it is advisable to consult a dermatologist or healthcare professional for proper evaluation and management.
| Signs of Severe Angular Cheilitis | How to Prevent Angular Cheilitis |
|---|---|
| Excessive redness | Maintain good oral hygiene |
| Swelling | Avoid excessive lip licking |
| Bleeding | Use lip balms with SPF |
| Difficulty in opening the mouth | Address underlying conditions |
When to seek emergency medical care for Angioedema
Emergency medical care may be necessary for angioedema if there is severe swelling that affects the airway, causing difficulty breathing or swallowing. In such cases, it is crucial to seek immediate medical attention at the emergency room. When faced with angioedema, it is important to understand when urgent care is required. Here are five signs indicating the need for an immediate visit to the emergency room:
- Severe swelling of the face, lips, tongue, or throat
- Difficulty breathing or shortness of breath
- Rapid onset of symptoms after exposure to a known allergen
- Hoarseness or difficulty speaking
- Swelling in areas such as the hands, feet, or genitals
Recognizing these symptoms and seeking prompt medical attention can help prevent potential complications and ensure appropriate management of angioedema. Remember that any concerns regarding your health should be addressed by a healthcare professional.
Prevention Methods
Prevention methods for both angular cheilitis and angioedema involve maintaining proper oral hygiene and avoiding triggers such as allergens or irritants. To prevent the recurrence of angular cheilitis, it is essential to keep the corners of the mouth clean and dry. Regularly washing the affected area with a mild soap and warm water can help remove any bacteria or fungi that may contribute to the condition. It is also important to keep the lips moisturized using lip balm or petroleum jelly to prevent dryness and cracking.
In addition to maintaining good oral hygiene, there are several home remedies that may help alleviate symptoms and prevent recurrence of angular cheilitis. Applying a thin layer of antifungal cream or ointment, such as clotrimazole, can help treat fungal infections that may be causing the condition. Aloe vera gel, known for its soothing properties, can also be applied topically to reduce inflammation and promote healing.
For angioedema prevention, identifying and avoiding triggers is crucial. Common triggers include certain foods (such as shellfish, nuts, or eggs), medications (like nonsteroidal anti-inflammatory drugs), insect bites or stings, latex products, and environmental factors (such as pollen or pet dander). Keeping a food diary can help identify specific food triggers in cases where angioedema is suspected to be caused by an allergic reaction.
While prevention methods are beneficial in managing these conditions, it is important for individuals experiencing recurrent episodes of angular cheilitis or angioedema to consult with a healthcare professional for proper diagnosis and treatment options. Dermatologists can provide personalized advice on preventive measures based on an individual’s specific condition and medical history. By following these preventative measures under medical guidance, individuals can reduce the frequency and severity of their symptoms while improving their overall quality of life.
Potential Complications
One important consideration when dealing with both angular cheilitis and angioedema is the potential complications that can arise from these conditions. Angular cheilitis, also known as perleche, is a common inflammatory condition characterized by cracks or fissures at the corners of the mouth. If left untreated, it can lead to secondary bacterial or fungal infections, causing further discomfort and prolonging the healing process.
On the other hand, angioedema involves localized swelling of deeper layers of skin and mucous membranes. It can occur in various parts of the body, including the lips, face, throat, and genitals. In severe cases, angioedema may obstruct the airway or cause anaphylaxis, a life-threatening allergic reaction.
To provide a clear understanding of potential complications associated with angular cheilitis and angioedema, let us consider them side by side in a table:
| Complications | Angular Cheilitis | Angioedema |
|---|---|---|
| Secondary infections | Bacterial or fungal infections may develop | Risk of infection due to breaks in skin integrity |
| Pain/discomfort | Cracks/fissures at mouth corners cause pain | Swelling can result in pain or discomfort |
| Impaired eating/speech | Difficulty chewing/swallowing/talking | Swelling may affect oral functions |
| Emotional impact | Self-consciousness due to visible symptoms | Anxiety/stress related to recurrent episodes |
Management strategies for these complications include maintaining good oral hygiene for angular cheilitis patients and avoiding triggers such as certain medications or allergens for those with angioedema. Prompt treatment with antifungal creams or antibiotics may be necessary for angular cheilitis-related infections. In severe cases of angioedema leading to airway compromise or anaphylaxis, immediate medical attention, including the administration of epinephrine and antihistamines, is crucial.
In conclusion, understanding the potential complications associated with angular cheilitis and angioedema is essential for effective management. By addressing these complications proactively and seeking appropriate medical care when needed, individuals can minimize the impact of these conditions on their daily lives.
Conclusion and Takeaways
In conclusion, understanding the potential complications and management strategies for angular cheilitis and angioedema is crucial in order to minimize their impact on individuals’ daily lives. These conditions may cause discomfort, pain, and embarrassment, leading to a decreased quality of life. By recognizing the key differences between angular cheilitis and angioedema, healthcare professionals can provide more accurate diagnoses and tailored treatments.
- Angular cheilitis is characterized by redness, cracking, and inflammation at the corners of the mouth. It is often caused by factors such as moisture buildup, nutritional deficiencies, or fungal infections. On the other hand, angioedema involves swelling beneath the skin’s surface and commonly affects areas like the lips, eyes, or throat. Allergic reactions or genetic factors are often responsible for its development.
- Treatment options for angular cheilitis include topical antifungal creams or ointments to address any underlying infection, as well as measures to keep the affected area dry and protected from further irritation. In contrast, angioedema management focuses on identifying triggers and avoiding allergens when possible. Antihistamines or corticosteroids may be prescribed to reduce swelling during acute episodes.
- It is essential for healthcare providers to approach patients with empathy when discussing these conditions due to their potential impact on self-esteem and social interactions. Providing education about proper hygiene practices, nutrition recommendations for angular cheilitis prevention or management of allergies in angioedema can empower individuals to take control of their condition.
By summarizing these key differences between angular cheilitis and angioedema accurately while considering patient-centered care principles throughout diagnosis and treatment plans can be individualized effectively. This comprehensive approach will enable individuals dealing with these dermatological conditions to better manage symptoms while improving their overall well-being.
Frequently Asked Questions
Can angular cheilitis and angioedema occur simultaneously?
Angular cheilitis and angioedema can occur simultaneously, although they are distinct conditions with different causes and treatments. Angular cheilitis is characterized by inflammation and cracking at the corners of the mouth, while angioedema refers to swelling beneath the skin’s surface. Both conditions can cause discomfort and affect one’s quality of life. Treatments for angular cheilitis may include topical creams or ointments, while angioedema may be managed with antihistamines or corticosteroids. Proper diagnosis by a healthcare professional is essential for effective management of these conditions.
Are there any specific risk factors for developing angular cheilitis?
Specific risk factors for developing angular cheilitis include a weakened immune system, nutritional deficiencies (such as iron or vitamin B12 deficiency), and poor oral hygiene. Other contributing factors may include wearing ill-fitting dentures, excessive saliva production, and frequent lip licking. These factors can create an environment that allows for the overgrowth of bacteria or fungi in the corners of the mouth, leading to the development of angular cheilitis. Taking steps to address these risk factors can help prevent or manage this condition effectively.
Can angioedema be caused by an allergic reaction?
Angioedema can be caused by allergic triggers, such as certain foods, medications, or insect bites. Common symptoms of angioedema include swelling of the deep layers of the skin, particularly around the eyes and lips. It can also affect the throat and cause difficulty in breathing. Prompt medical attention is necessary in severe cases to prevent complications. Treatment options may include antihistamines, corticosteroids, or epinephrine depending on the severity and underlying cause of angioedema.
How long does it typically take for angular cheilitis to heal?
The healing time of angular cheilitis can vary depending on the severity and cause of the condition. In most cases, it typically takes about 1 to 2 weeks for angular cheilitis to heal with proper treatment. Treatment options may include keeping the affected area clean and dry, applying topical antifungal or antibiotic creams, using over-the-counter lip balms, avoiding irritants, and addressing underlying factors such as nutritional deficiencies or denture-related issues. Seeking medical advice is recommended for an accurate diagnosis and appropriate treatment plan.
Are there any long-term complications associated with angioedema?
Long-term complications associated with angioedema can vary depending on the underlying cause and severity of the condition. In some cases, recurrent episodes of angioedema can lead to significant swelling and inflammation that may result in airway obstruction, posing a risk to breathing. However, with appropriate treatment options such as antihistamines, corticosteroids, or immune-modulating medications, these complications can often be managed effectively. It is important for individuals experiencing angioedema to seek medical attention and follow up with their healthcare provider for proper diagnosis and treatment.
Conclusion
Angular cheilitis and angioedema are two distinct dermatological conditions that can cause discomfort and affect individuals’ quality of life. Angular cheilitis is characterized by inflammation and cracking at the corners of the mouth, while angioedema involves swelling in deeper layers of the skin. These conditions differ in terms of location, appearance, duration, causes, and triggers. It is crucial to seek medical attention for proper diagnosis and treatment. Prevention methods can also be employed to minimize the risk of recurrence. While complications are rare, it is essential to be aware of potential complications associated with these conditions. In conclusion, understanding angular cheilitis and angioedema allows individuals to take appropriate measures for management and prevention.
Parallelism: Understanding angular cheilitis and angioedema’s differences in location, appearance, duration, causes, triggers; seeking medical attention for diagnosis; employing prevention methods; being aware of potential complications – all contribute to effective management and prevention strategies for these dermatological conditions.